Did you know research has shown the risk of getting type 2 diabetes is nearly 10 times higher for women who have had gestational diabetes during pregnancy (compared to women who have not had gestational diabetes)?
The SWEET Study is a research study to learn if a once-a-week medicine, called Ozempic, can help women get rid of prediabetes and have healthy blood sugar levels after a pregnancy with gestational diabetes.
SWEET Study participant Erica is sharing her journey through the SWEET Study in hopes that those who may qualify may join her on a health journey. Learn more about the study or see if you qualify by clicking here.
Week of April 1 – Meet Erica!
Well, hey! My name is Erica and I am participating in the SWEET Study at Woman’s Hospital.
What is the SWEET Study, you ask?
In layman’s terms, this is a study for women with pre-diabetes who recently had gestational diabetes to see if a medicine called semaglutide (Ozempic) can normalize blood sugars and prevent type 2 diabetes. The study takes up to eight months to complete and follows some women on active Ozempic and some on a placebo. The fun part is that neither the test subjects nor the research team will know if the participant will receive the placebo. In the end, researchers will compare the results of the two test groups to show whether Ozempic is successful in helping control the blood sugar of this particular group of women.
I received my first batch of injections on Monday, March 20!
Follow me to hear all about my experience in this trial and how my journey is going.
Let the adventure begin!
Week of April 10 – The SWEET Screenings
Let’s start from the beginning.
How did I learn about the study and the screening process?
The first qualification to participate in the SWEET Study is having had gestational diabetes during at least one pregnancy. I had it with both of my pregnancies and was prescribed Metformin to control my insulin levels. I wouldn’t call either of my pregnancies fun, but it was beyond worth it for my beautiful family.
The first time I heard about this study was through an email from Woman’s Hospital. I had signed up for notifications for research participation opportunities in the past, hoping to make some extra cash. When I read the description of the study and the required criteria that the participants needed to meet, it described the perfect chance for me to help make a difference — and of course, the extra cash didn’t hurt.
Another qualification to participate in the study is that you cannot be breastfeeding. When I first found out about the study in July 2021, I was still exclusively pumping for my son Ezra, so that first screening call ended quickly.
On Jan. 23, 2022, I spoke with Bri on the research team, and we set up my first screening visit. I got off of Metformin which took four weeks to “wash” off. Currently, I am on birth control and Effexor which are both approved to take while participating in the study. In fact, birth control is very important as they do not know the impact that Ozempic has on pregnancy.
Screenings:
February 20, 2022 – Initial Screening via Phone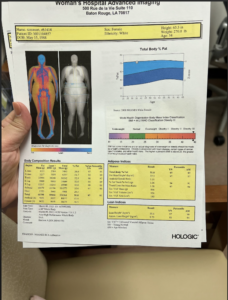
Bri went over the informed consent form with me, which is a full breakdown of how every visit will go and what will be expected of me throughout the study. Additionally, she also shared the benefits that the results of this study could provide. This is when I started thinking about why I should be a test subject for this research.
Facts I Learned About Gestational Diabetes:
- Women who experience gestational diabetes have a much higher chance of developing type 2 diabetes.
- That chance grows with each affected pregnancy.
Researchers’ Goals:
- The researchers hope to show that Ozempic can help maintain healthy sugar levels in these mothers.
My Fears for the Trial:
- Concerns about whether I’ll be able to be consistent & stick with it for such a long stretch of time.
- I don’t want to disappoint anyone or stretch myself too thin.
- I had also heard about some of the difficult side effects of Ozempic and worried about how that will affect my ability to function as a mom and employee at full capacity.
Ultimately, I prayed hard about it and felt this was an opportunity for myself and many mothers to come to be the best version of ourselves!
My Hopes for the Trial:
- The possibility of having extra help to get my health in check, plus making some extra cash, was the biggest motivator to be involved.
- This is my chance to do something for myself. I want to be healthy and feel good to enjoy this life with my kids!
- Helping mothers live longer, healthier, more active lives for their children was an opportunity I felt blessed to be a part of.
I couldn’t care less what size clothes I’m in, because let’s be honest: I’m fine no matter what. But I’m tired, I ache and I probably couldn’t go down a water slide without reaching 88mph!
First in-person Screening
After Bri went over the consent form, she took down my weight, height, and blood pressure. She checked each measure two to three times. We went down to the lab, where I felt like I had a Disney FastPass, and had a small amount of blood pulled to test my A1C and thyroid, kidneys, and liver functions.
Second in-person Screening
It was the dreaded glucose test. The full-blown, fasted, two-hour glucose test. I’ll probably never drink orange soda again! Bri and I went over a little medical history and she took my weight again. This part of the screening is what determines if I qualify for pre-diabetes and consequently dictates if I completely qualify to join the study. Turns out your girl is pre-diabetic and an official participant in the SWEET Study!
What’s a baseline visit?
This visit includes an approving doctor going over my medical history, to give his blessing on my joining the study. This doctor happens to be Dr. Neil Chappell, who is the medical monitor working on the SWEET Study. He is also a fertility doctor with Fertility Answers and is delightful. He is as brilliant as his bedside manner and humor.
Following my baseline visit, I did a full body composition scan (called a DXA) that is mostly used for finding out patients’ bone density but can also give body fat percentage data. I learned I am 51% fat. Yay me!
My final stop during this visit was with a registered dietitian to have a continuous glucose monitor attached to my stomach. I wore this device for 10 days before starting the injections and I will again after completing the study. This will give the research team data to compare how my body handles regulating my blood sugar before and post-study. Periodically, Bri will ask for a dietary recall of the last 24 hours. This will happen every once in a while throughout the eight-month study period. Although there is some accountability with that piece, Bri definitely did not make me feel bad about my eating habits! I think of it as her setting me up for success.
I hope you continue to follow my journey as I begin the process of administering my own injections.